Parkinson Pathfinder
Stay up to date with the latest at APDA Northwest by reading our Parkinson Pathfinder newsletters.
Read The Latest Parkinson Pathfinder
Spring 2025
Fall 2024
Summer 2024
Spring 2024
Fall/Winter 2023
Summer 2023
Spring 2023
Fall/Winter 2022
Summer 2022
Spring 2022
Winter 2021
Previous Newsletters
Fall 2021
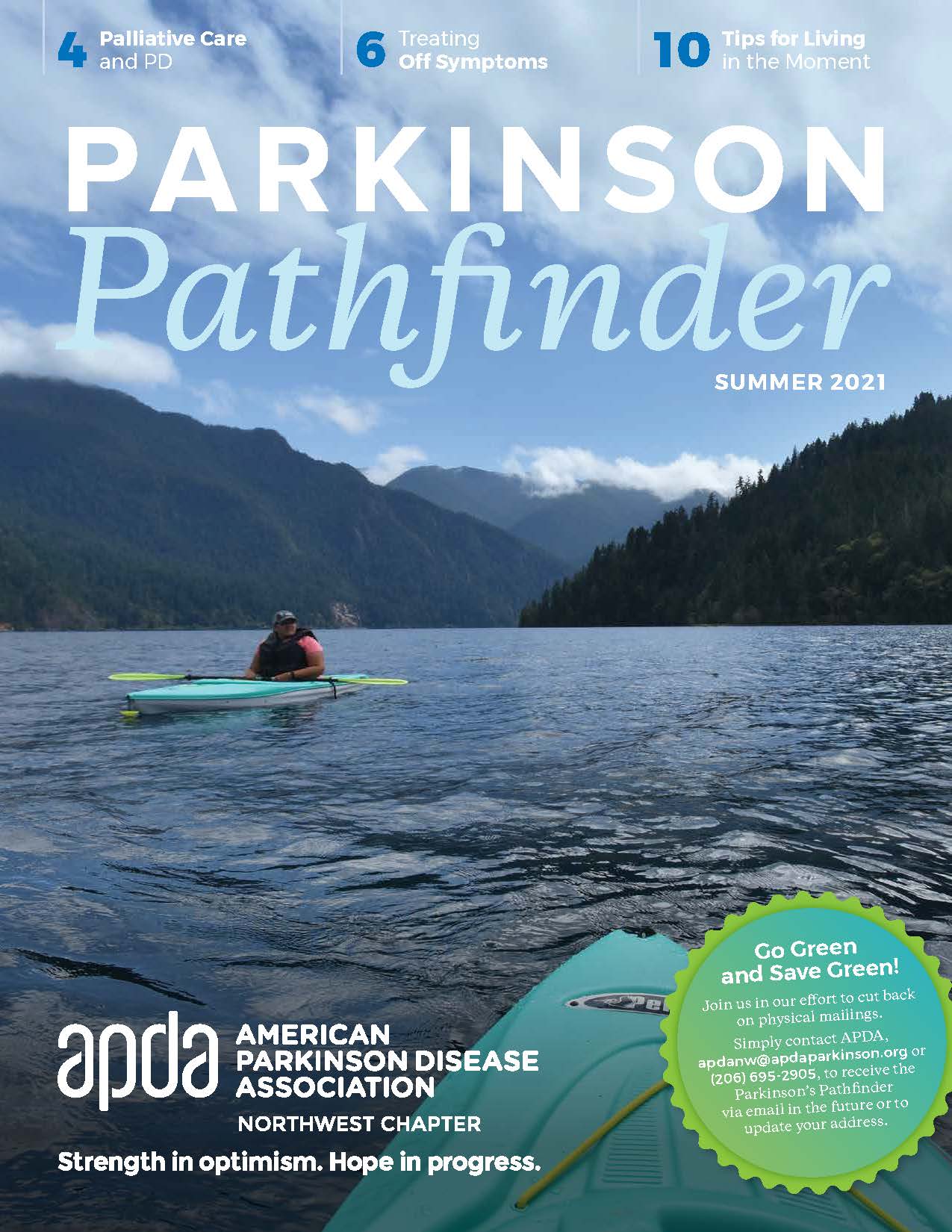
Summer 2021
Spring 2021
Winter 2020
Summer 2020
Spring 2020
Winter 2019
Fall 2019
Summer 2019
Fall 2018
Summer 2018
SPRING 2018
Summer 2017
FALL 2017
Spring 2017
Winter 2017
Summer 2016
| Other Past Newsletters |
|---|
| Spring 2015 |
| Winter 2014 |
| Fall 2014 |
| Summer 2014 |
| Spring 2014 |
| Fall 2013 |




