Parkinson’s Disease and Dyskinesia
If you have Parkinson’s disease (PD), there is a good chance that you’ve been, or will be taking medication containing levodopa. Levodopa is administered in combination with the drug carbidopa (Sinemet® and its generic versions). This drug combination is considered standard treatment for PD symptoms such as tremor, muscle stiffness, and slowness of movement. A side effect of long-term use of levodopa is dyskinesia. Learn more about dyskinesia, what causes it, how it can be managed, and some basic coping strategies below.
Watch Our Webinar: Spotlight on Dyskinesia and Off – Feeling Good Every Day
Speaker: Rebecca Gilbert, MD, PhD
Vice President, Chief Scientific Officer
American Parkinson Disease Association
What is dyskinesia?
The features of dyskinesia include rapid, involuntary, and uncontrollable movements other than tremor that present as body swaying, writhing (continual twisting, squirming, or contortions of the body), arm flailing, fidgeting, or head bobbing. Dyskinesia initially appears on the side of the body worst affected by PD. Although it can be localized to one part of the body such as the legs and arms, it can also spread to the torso, head, and neck. In rare circumstances, dyskinesia can also affect speech as well as respiratory and eye muscles.
Download our Dyskinesia Factsheet
What causes dyskinesia?
Dyskinesia is a side effect of long-term use of levodopa. The underlying cause of dyskinesia is complex and is not completely known. Normal brain function depends on a complex network of cells that communicates and functions via an array of different brain chemicals. One of these chemicals is dopamine. In PD, there is a loss of brain cells called dopaminergic neurons that make dopamine; therefore, the level of dopamine in the brain starts to decrease.
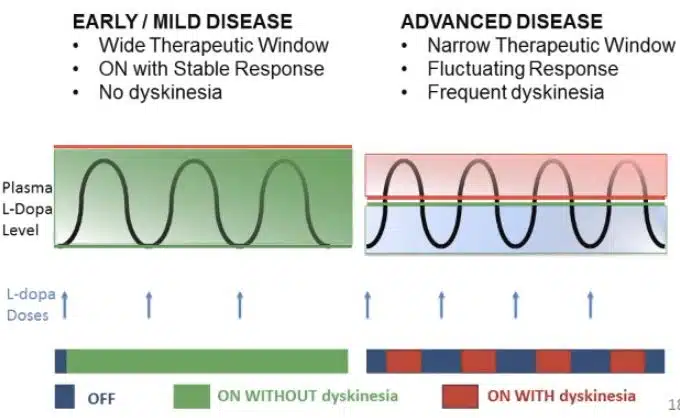
The purpose of taking levodopa is to temporarily restore the dopamine that is lost. However, since levodopa is intermittently taken over the course of a day, the level of dopamine will rise and fall. These dopamine level fluctuations, in combination with the loss of dopaminergic neurons, are thought to cause dyskinesia. Dyskinesia can occur when the level of levodopa in the body is at a maximum, referred to as peak dose dyskinesia, or when the levels of levodopa are rising or falling, referred to as diphasic dyskinesia.
If levodopa causes dyskinesia, then why should I take it?
At present, treatment with levodopa is the most effective way to relieve tremor, stiffness, and slow movement associated with PD. In the early stage of PD, levodopa may not be necessary and there are other medications available to treat this stage of the disease. However, as the disease progresses and its symptoms interfere with daily living, your doctor will prescribe levodopa. It’s important to note that there is a time lag of roughly four to ten years from the start of treatment with levodopa to when dyskinesia emerges, and its severity will vary among different individuals.
People who get PD in their later years (70 years and older) may not show signs of dyskinesia or may have only mild symptoms within their lifetime. Being diagnosed with PD at a younger age (40–59 years), also known as early onset PD or young onset PD, is associated with a greater chance of developing dyskinesia because these individuals will take levodopa for a longer period of time. Dyskinesia in its milder form may not be bothersome, and the mobility afforded by taking levodopa may be preferable to the immobility associated with not taking levodopa. People with PD must weigh the benefits of using levodopa versus the impact of dyskinesia on their quality of life.
Are there resources to learn more about dyskinesia?
APDA provides information, education, and support to those impacted by Parkinson’s disease and funds scientific research into the causes, prevention, and treatments.
Check out our resources about levodopa and dyskinesia that may be helpful:
Are there ways to manage dyskinesia?
Once dyskinesia has started it is difficult to treat. However, there are several ways to delay it from starting or reducing it once it has begun:
- If you have early onset PD with mild symptoms but do not yet have dyskinesia, your doctor may prefer to begin your PD treatment with drugs known as dopamine receptor agonists instead of levodopa. However, at some point these drugs will cease to be sufficiently effective and levodopa will be needed.
- Once dyskinesia has started and begins to interfere with daily life, your doctor may lower the dosage and adjust the time at which carbidopa-levodopa is taken, prescribe an extended-release formulation of this drug combination (Rytary®), or recommend continuous intestinal infusion of carbidopalevodopa (Duopa™). These treatment strategies may help reduce fluctuations in dopamine that contribute to dyskinesia.
- The drug amantadine can reduce dyskinesia and can also help PD symptoms. Amantadine (Symmetrel®) can be taken in multiple daily doses or in an extended-release formulation (Gocovri™) that maintains a high level of amantadine in the body throughout the day and has shown good results in reducing dyskinesia. In addition, the extended-release formulation taken orally – once at bedtime – may be more advantageous to some people than the multiple daily doses of immediate-release amantadine.
- Deep brain stimulation is a surgical method that can be used for severe symptoms of dyskinesia. It has been shown to be remarkably effective in carefully selected patients. There are very specific criteria for this procedure to be effective and is only done when other methods have not worked.
Are there coping strategies for living with dyskinesia?
There are several ways to manage dyskinesia and PD in general by incorporating some basic routines into your lifestyle.
- Keep a diary that logs the time and frequency of dyskinesia, which will help your doctor assess if your medications are working and help you schedule daily activities when mobility is better. The APDA Symptom Tracker app can help you keep track of a wide range of motor and non-motor PD symptoms, including dyskinesia.
- Physical activity, including mild aerobic exercise such as walking, dancing, and swimming, will help keep the body strong and prevent muscle weakening.
- Stress can make dyskinesia symptoms worse, so find ways to reduce stress (breathing exercises, massage, yoga, etc) and try to keep a positive attitude.
- Poor sleep at night is associated with dyskinesia. Aim for good sleep quality and try to experiment with different positions in bed that will help you relax and sleep better.

Explore Our New Parkinson’s Resource Library
Whether you are living with PD, caring for someone with PD, or are just looking for information, check out our new resource library to see articles, videos, webinars, and more in-depth information about Parkinson’s disease.

